Malaria: Understanding The Symptoms, Treatment, And Prevention
Posted Date: March 13th, 2023
Malaria is a serious and in some cases perilous sickness brought about by a parasite called Plasmodium which is communicated to people through the chomp of a tainted female Anopheles mosquito.
There are such Plasmodium parasites that can cause malaria fever in people, yet the most outstanding and harming species are Plasmodium falciparum and Plasmodium vivax.
Jungle fever is a significant general medical condition in many regions of the planet, especially in sub-Saharan Africa where it is liable for countless passings especially among small kids.
In any case the sickness likewise happens in different regions of the planet including Asia, Latin America and portions of the Center East.
Symptoms of Malaria
The side effects of jungle fever can differ contingent upon the types of Plasmodium parasite causing the contamination as well as the singular’s safe framework and different variables. Certain individuals might not have any side effects whatsoever, while others might encounter extreme side effects that require hospitalization.
The typical symptoms of malaria include:
1. Fever: A high fever is often the first sign of malaria and it can come and go in cycles that last 6 to 12 hours.
2. Chills: Patients with malaria may experience sudden coldness and shivering, followed by a high fever.
3. Headache:A severe headache is a common symptom of malaria and it can be accompanied by other neurological symptoms such as confusion, seizures and coma in severe cases.
4. Muscle and joint pain: Malaria can cause muscle aches and pain as well as joint pain and swelling.
5. Fatigue: Many people with malaria experience extreme tiredness and weakness and they may have difficulty performing even simple tasks.
6. Nausea and vomiting: Some people with malaria may experience nausea and vomiting, particularly during the initial stages of the illness.
7. Anemia: Malaria fever can cause sickliness a condition in which the body has less red platelets than ordinary, prompting weariness and shortcoming.
If left untreated, malaria can progress rapidly and cause serious complications such as organ failure and even death. It is important to seek medical attention promptly if you experience any of these symptoms, particularly if you have recently traveled to an area with a high risk of malaria transmission.
Causes of Malaria
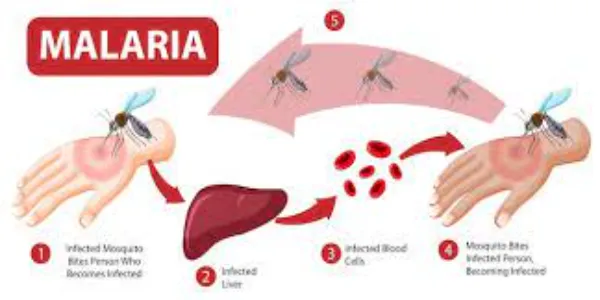
Malaria is caused by the transmission of the Plasmodium parasite from an infected female Anopheles mosquito to a human host. At the point when a tainted mosquito nibbles an individual, it infuses the parasite into the individual’s circulation system.
The parasite then goes to the liver where it duplicates and at last reenters the circulation system where it contaminates and annihilates red platelets.
There are four kinds of Plasmodium parasites that usually cause wilderness fever in individuals: Plasmodium falciparum, Plasmodium vivax, Plasmodium malariae and Plasmodium ovale.Plasmodium falciparum is the most dangerous species and answerable for most of intestinal
Sickness related passings around the world.
The gamble of contracting jungle fever is most noteworthy in regions with high paces of transmission, especially sub-Saharan Africa where Plasmodium falciparum is the most common species. Malaria transmission rates can also be influenced by factors such as climate, mosquito control measures and the behavior of the mosquito vector.
Not with standing mosquito chomps, jungle fever can likewise be communicated through blood bondings, organ transfers and shared utilization of needles or needles tainted with contaminated blood. However these modes of transmission are relatively rare compared to mosquito bites.
It is important to note that malaria is not a contagious disease and cannot be spread from person to person through casual contact or respiratory droplets.
Diagnosis of Malaria
The diagnosis of malaria involves several steps including a physical exam, medical history and laboratory tests. Since the side effects of jungle fever can be like those of different diseases, it is vital to affirm the analysis with research center tests.
The following are some common diagnostic methods for malaria:
1. Blood smear: This is the most commonly used method for diagnosing malaria. A small sample of the patient’s blood is placed on a slide and examined under a microscope to look for the presence of the Plasmodium parasite in red blood cells.
2. Rapid diagnostic test (RDT): RDTs are available as kits and use a small drop of blood from a finger prick to detect specific proteins produced by the Plasmodium parasite.
3. Polymerase chain reaction (PCR): PCR is a highly sensitive diagnostic test that can detect even small amounts of the parasite’s DNA in blood samples.
4. Serology: This involves testing a patient’s blood for antibodies to the Plasmodium parasite. This method is not commonly used for diagnosis because antibodies can persist in the blood long after the infection has cleared.
It is important to diagnose and treat malaria promptly to prevent complications and reduce the risk of transmission to others. Assuming you suspect that you have jungle fever, it is vital to look for clinical consideration from a medical care supplier with experience in diagnosing and treating the illness, especially assuming you have as of late gone to a region with a high gamble of jungle fever transmission.
Treatment of Malaria
The treatment of malaria depends on several factors including the species of Plasmodium parasite causing the infection the severity of symptoms the patient’s age and health status and the presence of any other medical conditions. In general the goals of treatment are to eliminate the parasite from the bloodstream, prevent the development of complications and reduce the risk of transmission to others.
The following are some common medications used to treat malaria:
1. Artemisinin-based combination therapies (ACTs): ACTs are the preferred treatment for uncomplicated malaria caused by Plasmodium falciparum which is the most deadly species. ACTs are highly effective and usually well-tolerated, but they can cause side effects such as nausea, vomiting and diarrhea.
2. Chloroquine: Chloroquine is an older medication that is effective for treating malaria caused by Plasmodium vivax and Plasmodium malariae, but it is no longer effective against Plasmodium falciparum in many areas due to the development of drug-resistant strains.
3. Quinine: Quinine is a medication used to treat severe malaria caused by Plasmodium falciparum and it is often used in combination with other medications.
4. Atovaquone-proguanil: This medication is effective for treating malaria caused by multiple species including Plasmodium falciparum and it is often used for prophylaxis in travelers to areas with high rates of transmission.
In addition to medications, patients with malaria may also require supportive care to manage symptoms and prevent complications. This may include hydration with fluids and electrolytes, treatment for anemia and management of any other medical conditions that may be present.
It is important to follow the healthcare provider’s instructions for taking medications and to complete the full course of treatment, even if symptoms improve before the medication is finished. Failure to complete the full course of treatment can lead to a relapse of the infection and increase the risk of drug resistance.
Prevention of Malaria
1. Preventing malaria involves a combination of measures that target both the mosquito vector and the human host. The following are some common methods of malaria prevention:
2. Mosquito control: Mosquito control measures can help to reduce the population of Anopheles mosquitoes which are the primary vector for malaria transmission. These measures may include insecticide-treated bed nets, indoor residual spraying and environmental management to eliminate breeding sites.
3. Chemoprophylaxis: Chemoprophylaxis involves taking medication to prevent malaria before, during and after travel to areas with a high risk of transmission. The type of medication used and the duration of treatment may vary depending on the destination and the traveler’s age and health status.
4. Personal protection: Personal protection measures can help to reduce the risk of mosquito bites and include wearing long-sleeved clothing and pants, using mosquito repellent and staying indoors during peak mosquito activity.
5. Early diagnosis and treatment: Early diagnosis and treatment of malaria can prevent the development of severe symptoms and reduce the risk of transmission to others.
6. Vaccination:Currently there is only one malaria vaccine available, known as RTS,S. This vaccine has been shown to provide partial protection against Plasmodium falciparum in children in sub-Saharan Africa.
7. It is important to consult with a healthcare provider before traveling to areas with a high risk of malaria transmission to determine the most appropriate prevention measures. Travelers should also stay informed about the risk of malaria in the area they are visiting and take steps to prevent mosquito bites and seek prompt medical attention if they develop symptoms of malaria.
Complications of Malaria
Malaria can lead to a variety of complications, particularly if left untreated or if the infection is caused by a more severe species of Plasmodium parasite. Some common complications of malaria include:
1. Anemia: Malaria can cause a destruction of red blood cells which can lead to anemia. Symptoms like fatigue, weakness and shortness of breath can be caused.
2. Cerebral malaria: This is a severe form of malaria that affects the brain and can cause seizures, coma and even death. Cerebral malaria is most commonly caused by Plasmodium falciparum.
3. Acute respiratory distress syndrome (ARDS): ARDS is a serious complication that can occur in severe cases of malaria, particularly in children. It can lead to respiratory failure and requires immediate medical attention.
4. Organ failure: In severe cases of malaria, multiple organ failure can occur including liver and kidney failure.
5. Hypoglycemia: Malaria can cause a drop in blood sugar levels which can be life-threatening, particularly in children.
6. Recurrence: Malaria can recur even after successful treatment if the parasite persists in the liver or if the patient is re-infected.
It is important to seek prompt medical attention if symptoms of malaria occur, particularly if traveling in areas with a high risk of transmission. Early diagnosis and treatment can help to prevent complications and reduce the risk of transmission to others.
Malaria in different parts of the world
Malaria is a major public health concern in many parts of the world, particularly in sub-Saharan Africa, Southeast Asia and South America. The following are some examples of the prevalence of malaria in different regions:
1. Sub-Saharan Africa: Sub-Saharan Africa bears the highest burden of malaria cases and deaths, accounting for 94% of malaria cases and deaths worldwide. Children under the age 5 and pregnant ladies are mostly at risk.
2. Southeast Asia: Southeast Asia is also a high-risk region for malaria, with approximately 8% of the global malaria burden. Malaria is prevalent in rural areas, particularly in forested areas where Anopheles mosquitoes breed.
3. South America: Malaria is found throughout South America, but the incidence is highest in the Amazon region, particularly in Brazil, Colombia and Peru.
4. India: India is home to approximately 85% of malaria cases in the Southeast Asia region, with the majority of cases occurring in rural areas. Plasmodium falciparum is the most common species and drug-resistant strains are a concern.
5. Central America and the Caribbean: Malaria is less common in Central America and the Caribbean than in other regions, but transmission can occur in rural areas and during the rainy season.
It is important to be aware of the risk of malaria when traveling to areas with a high prevalence of the disease and to take appropriate prevention measures. Travelers should consult with a healthcare provider before traveling to determine the most appropriate prevention measures and to seek prompt medical attention if symptoms of malaria occur.
Conclusion: The Importance of Understanding Malaria
Malaria is a serious and potentially life-threatening disease that affects millions of people worldwide, particularly in sub-Saharan Africa, Southeast Asia and South America. It is caused by the Plasmodium parasite which is transmitted to humans through the bite of infected Anopheles mosquitoes.
Early diagnosis and treatment of malaria are critical to prevent complications and reduce the risk of transmission to others. Symptoms of malaria include fever, chills, headache and body aches which can often be mistaken for other illnesses.
Prevention measures include mosquito control, chemoprophylaxis, personal protection, early diagnosis and treatment and vaccination. It is important to consult with a healthcare provider before traveling to areas with a high risk of malaria transmission to determine the most appropriate prevention measures.
Understanding the prevalence of malaria in different parts of the world can help individuals make informed decisions about travel and take appropriate prevention measures. Increased awareness of malaria and its transmission can also help to reduce the global burden of the disease and improve public health outcomes.
Related Posts
Dr. Emily Carter is a seasoned health writer and wellness advocate at Healths News Today. With over a decade of experience in the healthcare industry, she specializes in translating complex medical information into easy-to-understand content that empowers readers to make informed decisions about their health.




